The reality of translating strategy into real change on the frontline during exceptional times
As healthcare professionals it feels as if we are being hit by a tsunami of information and change right now – there’s evolving leadership theory; developments in national & professional strategy; concepts of change; and challenges to delivering that change. This all comes on top of managing the impact of the pandemic and the stresses in just doing our day jobs. I’ve been reflecting on delivering change on the frontline in the clinical setting at the bedside, working with colleagues to see how we can deliver maximum benefit for both patients and clinicians.
This blog is based on a presentation given recently at the CHIME Digital Leadership Academy for Nurses and Midwives. It delves into my own experiences of facilitating change, from digging into the process of identifying the problem to be solved, through to defining and delivering success, and to reflecting on the ROI of investments in Healthcare IT.
Delivering change at a time of unprecedented challenges
Right across the spectrum from acute to community care, be that mental health or general healthcare, circumstances that would ordinarily have been demanding, have seen challenges increase exponentially over the last few years. Locally, regionally, nationally and globally it’s become ridiculously complex to provide patient-centred care, while remaining highly adaptive, and while under enormous strains and pressures including:
- Patient load
- Bed capacity
- Staffing levels
- Ineffective communication
- Challenges to team working
These issues are straining our abilities to deliver patient-centric care, in a timely manner, while remaining compliant with procedures and processes. New technologies are playing an increasingly significant role at the point of care – but to be really helpful technology needs to be addressing the real issues we’re facing or it threatens to become just another burden.
Technology is evolving at an immense pace, with the power to catapult us from manual and paper processes to an increasingly automated and virtual world but all too often time is the limiting factor on success in adopting and adapting to technological advances.
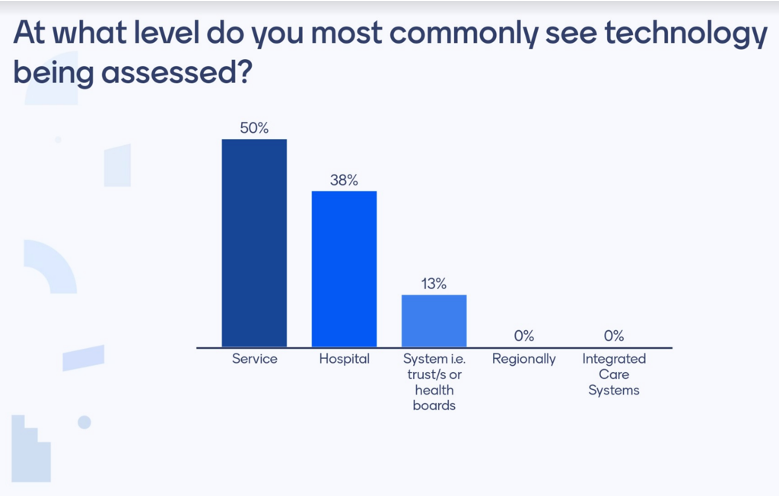
During the presentation we ran a poll that found 50% of the audience saw technology being assessed at the service level as opposed to 38% at Hospital level.
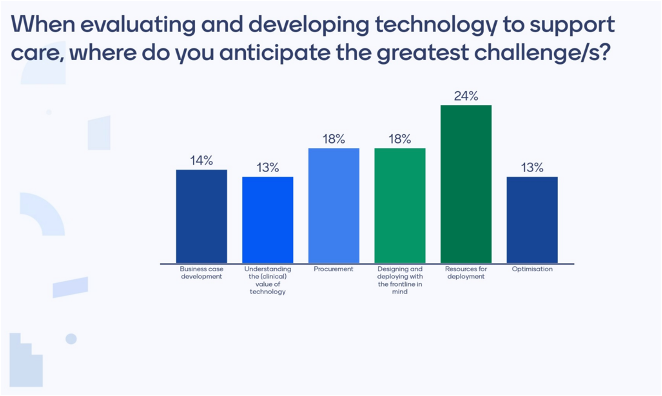
Survey respondents also saw the greatest technology challenges in finding Resources for Deployment (24%); Designing and Deploying with the Frontline in mind (18%); and Procurement (18%).
The key approaches which I find myself using again and again to successfully address these issues include:
- Setting SMART objectives (Specific; Measurable, Achievable; Realistic; Time-bound)
- Planning for joined-up outcomes
- Focusing on service design
- Considering change management
Setting realistic and measurable objectives
Defining SMART objectives has been a tried and tested approach which I have applied in staff development and performance management throughout my career. Here are some examples of applying the SMART approach to current healthcare challenges:
- Specific issues to be addressed include:
- Users challenged by complex access to systems, data and devices
- Time spent on repetitive, manual logins
- Interruptions to clinical workflows
- Overburdened helpdesk
- Need to increase EMR adoption
- Measurable improvements could include:
- Change in compliance to procedures
- Percentage reduction in helpdesk calls
- Time reduction in accessing systems
- Increase in productivity
- Achievable
- The goals set must provide tangible benefits AND be deliverable
- Impossible goals will act as a disincentive to make any change at all
- Realistic (and Relevant)
- The objectives set must be applicable to the audience
- Each person/team/department/organisation needs objectives which relate directly to them and to be able to see how their change objective can contribute to overall goals
- Time-bound
- Each goal must be tied to a time by which it must be delivered
Planning for joined-up outcomes
It is vital to connect the adoption of technology innovations to the demands of policy, practice and the real challenges faced in delivering care. National strategies and policies, regional practice, organisational specifics and service characteristics must be taken into account. It is no good in designing and implementing what seems a ‘perfect solution’ if it does not consider the wider picture including the patient experience; acceptability to staff; regulatory requirements; safeguarding; information governance; IT constraints… and more.
Focus on service design
The knowledge I have built up from multiple projects in different settings around the world is that an experience-based co-design approach to services is best. Placing and keeping patients at the centre of solution design is critical. The dimensions to this are safety; quality; experience; and efficiency.
It is especially important in time sensitive processes and treatment areas such as stroke care, cardiac, sepsis and trauma to keep patients at the heart of thinking and design, considering all the elements including triage, assessment, planning, implementation and evaluation of care.
Good service design can benefit from the adoption of appropriate technology advances which can increase efficiencies, improve patient and family experiences and create an environment that is reducing error and complications. The aim should be for healthcare providers to create a more conducive healing environment underpinned by a more supportive team environment.
Making change happen through proactive management
Organisational theorist Richard Beckhard said, “For change to happen, the forces for change must outweigh the perceived cost of change.” In the end realising change is all about people. So it is important to not forget the role of change management in delivering successful outcomes.
Visionary leaders paint the big picture of how a solution will be locally realised. First by defining and communicating the vision and end state, then by outlining the preparation, means of delivery and how value will be secured and maintained. It is also important to show how to maintain business continuity while adopting the needed innovations.
Stakeholder engagement and ongoing communication is important. It is vital to assess change readiness and resistance across the organisation and to tailor messages, goals, training and communications to specific groups and individuals accordingly.
Identifying and recording ROI
It is really important for projects to not only be perceived as successful but also to be able to show measurable benefits to prove success. To be able to achieve this you have to record the ‘as is’ situation before changes are designed and introduced so that you can show the changes made.
Brainstorming ROI ideas with a wide range of representatives who will have differing perspectives and provide valuable sources of different types of information is a good approach that helps to promote engagement. Both quantitative and qualitative measures should be explored. Quantitative ROI might include the dimensions of experience, safety and quality. Qualitative measures might include such things as the behavioural changes of clinicians; movement in perceptions through interviews and surveys; technology adoption and comfort levels with its use; improvements perceived in team work and morale.
In conclusion
Successful change doesn’t just happen, it has to be designed and planned with the people in mind who will be using the technology. Looking at my own variety of experience in different situations around the world in realising outcomes with patients and clinicians through the adoption of technology has emphasised this. It’s important to give ourselves the time to learn from a breadth of experiences of what’s worked and what hasn’t, especially at this time of unprecedented challenges coupled with amazing innovations made possible by new technologies.
To find out more and contribute to the debate, download the Imprivata White Paper “Change – It’s about Time”.
